What are we curious about?
Replicating complex human biology.
Remarkable advances in microphysiological systems technology and tissue engineering have opened up new possibilities to study human-specific biology and diseases. We are utilizing this progress to “humanize” medical research and develop approaches to mimic complex multiorgan physiology and systemic immunology.
Tissue homeostasis and regeneration.
Our early studies of ex-vivo multiorgan interactions show intriguing differences in tissue functionality and maturation when kept in isolation or in communication with other organs. We are interested to identify mediators responsible for this increased life-like behavior of various organ systems and contributors to their homeostasis to inform new paradigms in regenerative medicine.
Immunometabolism in health and disease.
We are passionate about understanding how fundamental disruption in tissue-tissue and tissue-immune crosstalk leads to the early emergence of immunometabolic and neurodegenerative disorders such as Inflammatory Bowel Disease, diseases of the liver and Parkinson’s disease. These remain some of the biggest challenges of our time.
Humanness and the pursuit of life
What does it mean biologically to be human and where does humanness start? As we are advancing human biomimetics and human-machine integration, these questions are as relevant as ever. We hope to contribute new theoretical concepts to the evolving notion of what biological life and being human means today and in the future.
Research
We study how human organs talk to each other—and how those conversations keep us healthy or push us toward disease. Our team builds linked, miniature organ models made from human cells to recreate gut, liver, lymph node, brain, and metabolic tissues from the same donor. Using multiomic endpoints and computational biology we are watching how signals move across these connected systems, we uncover root-cause mechanisms in immunity, neurodegeneration, and metabolism, and we turn those insights into better diagnostics and therapies.
Projects
Tissue-resident immune environments across multiple organ systems
We connect same-donor, engineered human gut, liver, and lymph node tissues—and pair them with single-cell profiling—to see how local tissue-resident immune cells sense microbes, diet, and injury, and how those signals propagate tolerance or trigger inflammation across organs. These linked models serve as personalized surrogates of individual responses to infection, autoimmunity, and cancer, revealing new roles for tissue-resident immunity and informing the design of better vaccines, biologics, and cell therapies.
Identifying immunometabolic modulators of neurodegenration in the Gut-Brain axis.
We engineer an all-human, same-donor gut–liver–brain circuit to resolve how peripheral metabolites and proteins reshape brain maturation and neuroinflammatory tone. By fluidically coupling intestinal epithelium and hepatocyte-like tissue to midbrain-patterned organoids (with microglia) and tracing factor transfer with targeted proteomics, we identify gut- and liver-derived drivers of Parkinson’s-relevant phenotypes that only emerge under inter-organ crosstalk. CNS drug failures often stem from models that ignore systemic context; our goal is to expose causal, human-specific pathways that de-risk targets before clinical translation.
Systemic metabolsim and ageing
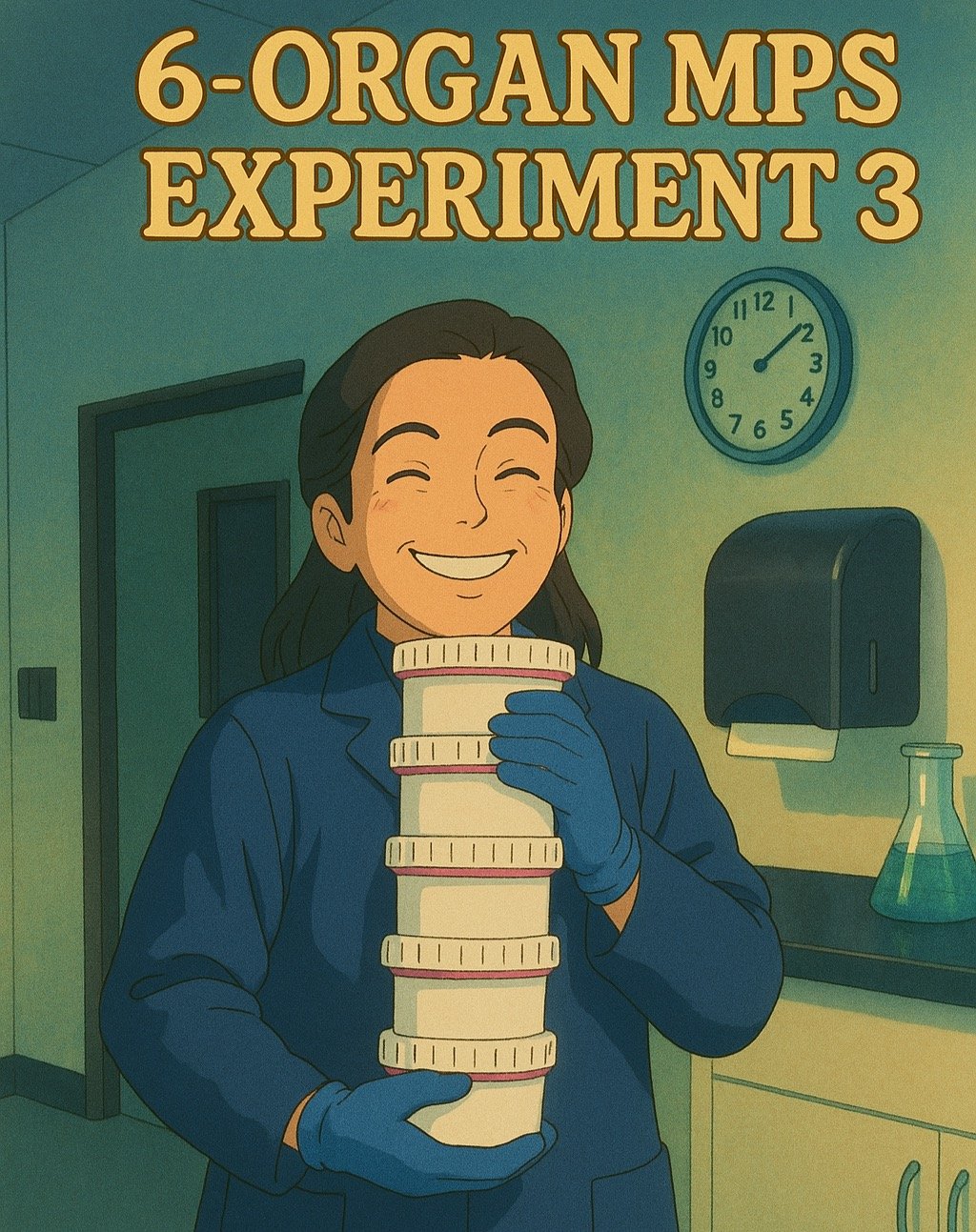
We integrate six donor-matched modules—gut, liver, pancreatic islets, skeletal muscle, adipose, and brain—perfused with circulating immune cells to quantify emergent control of glucose and lipids. Time-series multi-omics under fasting, normal, and “Western-diet–like” stresses train a computational digital twin that links metabolic decompensation to meta-inflammation and brain vulnerability, and benchmarks pharmacologic rescue (e.g., metformin, semaglutide). Metabolic homeostasis is an emergent network property; isolating organs hides failure modes that drive aging and neuro-inflammatory risk. We build the human in-vitro analogue needed to reveal—and reverse—those network collapses.
MicroPhysiological Systems
We engineer human multi-organ platforms purpose-built to expose interorgan causality. Our systems use modular, donor-matched compartments linked by a shared micro-circulation, with independently tunable flow, residence time, barrier function, and immune trafficking. Designs emphasize adaptability and adoption: interchangeable channel and floor geometries, standard lab interfaces (common pumps, tubing, plate-reader access), sampling ports for time-series multi-omics, footprints scalable from 2–8 tissues, and clear SOPs/BOMs so other groups can reproduce and extend the work. Most models optimize a single tissue and lose the cross-talk that drives real disease. We build tools that preserve each tissue’s ideal conditions while enabling controlled coupling and rigorous, sharable workflows—so the field can test causal hypotheses and translate findings faster.
What we strive for
Publications
Personalized Gut–Liver Microphysiological System Maps Donor-Specific Tissue-Resident Immunity and Reveals a Conserved Metabolic Crosstalk
Uslu et al., BioRxiv 2025
Multiorgan microphysiological systems as tools to interrogate interorgan crosstalk and complex diseases.
Trapecar, FEBS Letters 2021
Human physiomimetic model integrating microphysiological systems of the gut, liver, and brain for studies of neurodegenerative diseases
Trapecar et al., Science Advances 2021
Gut-Liver Physiomimetics Reveal Paradoxical Modulation of IBD-Related Inflammation by ShortChain Fatty Acids
Trapecar et al., Cell Systems 2020
Meet the Team
-

Martin Trapecar
PRINCIPAL INVESTIGATOR
-

Marissa McGilvrey
POSTDOCTORAL FELLOW
-

Shicheng Ye
POSTDOCTORAL FELLOW
-

Shereen Chew
PhD CANDIDATE
-

Andrea McPherson
RESEARCH SPECIALIST
-

Ronald Bronson
RESEARCH SPECIALIST
-
Lorenzo Thomas
PROGRAM COORDINATOR
Open positions
We are always looking to expand our team by creative, motivated and kind members. If interested in joining, please respond with a CV and description of scientific interests to mtrapec1@jhmi.edu.
Postdoctoral Fellow — Immune Cell Engineering for Pediatric Glioma
The Laboratory of Human Biomimetics (humanbiomimetics.com) at Johns Hopkins All Children’s Hospital / Institute for Fundamental Biomedical Research in St. Petersburg, FL is recruiting a creative, mission-driven Postdoctoral Fellow to help engineer next-generation immune therapies for pediatric glioma. Our group reverse-engineers multiorgan human biology using iPSC/organoids, microphysiological systems (MPS), fluidics, and systems biology to address hard problems in medicine.
In this role, you will integrate immune-cell and tissue engineering to build patient-specific multiorgan MPS that connect glioma, the blood–brain barrier, liver, and immune compartments. Using these living avatars, you will design, iterate, and test personalized cellular immunotherapies—optimizing efficacy, trafficking across the BBB, and safety liabilities such as cytokine release or hepatic off-targets. The position is highly collaborative, with direct access to clinicians and cross-disciplinary partners, and expects first-author manuscripts, conference presentations, and mentorship of junior trainees.
What we’re looking for. Prior, hands-on experience engineering immune cells—specifically CAR and/or TCR T cells—is required. You should bring a Ph.D. (or M.D./Ph.D.) in Immunology, Bioengineering, Cancer Biology, Synthetic Biology, or a related field; fluency with functional immunology (co-culture killing, cytokine profiling), molecular biology and vector design, and flow cytometry and imaging; and the ability to drive an independent project while thriving on teamwork and clear communication.
Great to have. We’re excited by candidates who have engineered NK cells or macrophages; built logic-gated/synNotch circuits or safety switches; used CRISPR (including base/prime editing); worked with brain tumor models, BBB systems, or patient-derived glioma lines; or have practical experience with microfluidics/organ-on-chip, 3D bioprinting, or biomaterials. Familiarity with iPSC differentiation (neural, endothelial/pericyte, hepatic) is helpful, as is comfort with multi-omics (scRNA-seq/spatial, proteomics/metabolomics) and analysis in R or Python. A translational mindset—thinking in terms of potency, QC, and GMP-relevant considerations—will set you apart.
Our environment. We’re based at a superbly equipped institute in St. Petersburg, Florida, with full access to resources at the Johns Hopkins Baltimore campus and a culture that prioritizes mentorship, career development, and a clear path to independence. St. Pete offers an outstanding quality of life: affordable living, beaches and nature, proximity to Tampa International Airport, and a vibrant cultural scene.
Appointment and application. Start date is flexible; applications are reviewed on a rolling basis. Salary and benefits are competitive and commensurate with experience, with Johns Hopkins benefits. To apply, send a single PDF containing (1) a cover letter describing your fit and your vision for immune engineering in pediatric glioma, (2) your CV, and (3) contact information for 2–3 references. Use the subject line “Postdoc — Immune Cell Engineering (Pediatric Glioma)” and submit via mtrapec1 (at) jhmi.edu.